Bonus Issue #03: FAQ's about Endometriosis + My Endo Surgery
Everything you need to know about Endo, FAQ's, and all about my Endo excision surgery + recovery.
This is a bonus issue of Sitting in a Tree, available to all paid and free subscribers, as I hope to shed more light on this misunderstood disease that affects 1 in 10 women.
Answering all the questions I very frequently get asked about my experience with Endometriosis, here, and please keep in mind that this is all my personal experience and information I’ve learned over the years— none of this is to be take as medical advice.
I’m currently exactly 3 weeks post-op from my first Endo excision surgery, so it feels like the perfect time to share this long-awaited bonus issue to answer all the FAQ’s I get about Endometriosis and my experience with it. This post shares more insight, but Endometriosis has infiltrated my life for the last four years. It isn’t just painful periods, and it is a wildly misunderstood, confusing disease; largely so, because women’s healthcare is woefully underfunded:
In 2022, research funding by the NIH (National Institutes for Health) for Endometriosis was $27 million. It was only $6M, as recently as 2017.
To put that into context, Diabetes got $1.1 billion in the NIH budget in the same year (2022). Diabetes is estimated to affect 37 million Americans.
The US population in 2022 was 333 million. Half the population being women (166.5 million), and Endo affecting 1 in 10 women, there’s approximately 16.65 million people with Endo. $27 million in funding for 16.65 million people, compared to another disease that got more than 4x that funding for only a little more than 2x people affected. That’s about 50% less funding per person affected by this disease.
What is Endometriosis?
Endometriosis is a disease, in which tissue similar to (but pathologically different than!) the tissue that lines your uterus (the endometrium) is found outside of your uterus in places it's not supposed to be— the tissue is most commonly found in the pelvis, ovaries, fallopian tubes, bowels, ureters, intestines, and can even be found on the appendix, esophagus, or other organs.
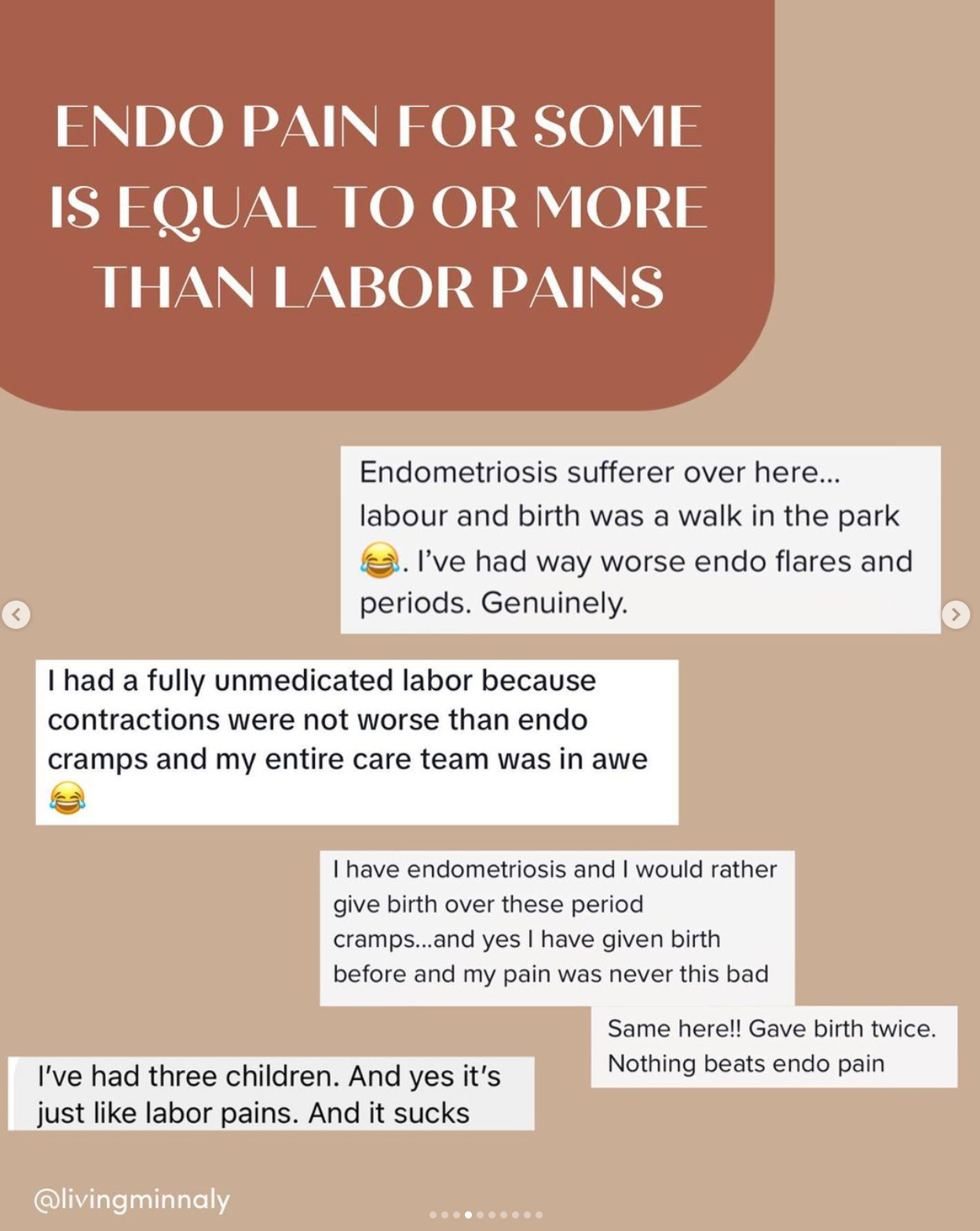
While symptoms and pain vary, Endometriosis can be extremely painful because the endometrial-like tissue acts similar to endometrial tissue with the hormonal menstrual cycle. And get this: endometriosis tissue makes it’s OWN hormonal production. With the development / spread of the disease and infiltration of the Endometriosis in the body, it can create scar tissue and adhesions, which can result in surrounding organs and pelvic tissue sticking together, creating extreme dysfunction and pain. Endometriosis can be extremely painful, life-disrupting, and is one of the leading causes of infertility.
If you are new to this disease, I HIGHLY recommend this comprehensive article that debunks many myths about Endo and the treatment for Endo.
Diagnosis
How do you get diagnosed for Endometriosis?
Endometriosis often does not show up on imaging, although MRI’s and ultrasounds are utilized by doctors to give them more insight on your case. For me personally, my MRI did not show anything except a retroverted uterus and compressed ovary, which indicated potential Endo adhesions. I also had a transvaginal ultrasound that gave me my first misdirected diagnosis of Adenomyosis (a sister disease to Endo).
Biopsy of excised Endo tissue during surgery is the only way to officially confirm diagnosis— this is why this disease makes insurance coverage so tricky (we’ll cover more on insurance below in the surgery section). BUT, an Endo specialist (not just your average OBGYN) can give you a strong idea of if your symptoms indicate likely possibility of the disease.
It takes an average of 7 years to reach a diagnosis of Endometriosis for many people, due to insufficient knowledge about it in the medical field, gaslighting (saying that period pains are just part of being a woman), and lack of awareness for this diseease.
Symptoms
What were your symptoms?
While symptoms can wildly vary from person to person with Endo, it is NOT just painful periods. My personal symptoms evolved over time and worsened with several of them: debilitating and heavy periods, ovulation pain, extreme pain when my bladder was full, pelvic floor dysfunction, occasional pain with sex (particularly with orgasm, which is just cruel?!) and then the more “discreet” symptoms were the parts I struggled to acknowledge most— I attributed my never-improving fatigue and brain-fog to being burned out and overcommitted, but this is very much my Endo. I also have several food intolerances (gluten and dairy) I attributed to my Hashimoto’s too, but it could be from both, there’s not a way to definitively know.
I also had very irregular cycles and heavy, clotty periods, but those two things were greatly helped by my addressing my overall hormonal health with some lifestyle and dietary management.
Management
How do you manage your Endo?
The gold standard of Endometriosis care is excision surgery (more on that below). Other methods include: OTC pain relief, acupuncture, pelvic floor therapy, dietary + lifestyle changes, hormonal treatment/BCP (although this is not a long-term solution and can cause more issues from some people)
Dietary adjustments: steering clear of foods that I know are inflammatory for me (gluten, dairy), and excess consumption of sugar, caffeine, and alcohol. None of those are fun answers and by no means will following a perfect diet magically siphon the Endo pain and symptoms away, however, for many people, you can find some improvements and relief in little adjustments. I personally notice a difference with alcohol, sugar, and caffeine intake levels… womp, womp.
TCM herbs: I use this company Elix’s personalized blend for me because they make it so easy (a lot of these herbs aren’t easy to track down individually)! This has made a difference in the regularity of my cycles and they’re far less heavy / clotty— TCM remedies like herbs and acupuncture do take time to take effect, and I started seeing improvements in my cycle with using Elix on my third cycle after starting . Use code MINNA20 for 20% off a 3-month intro bundle (this isn’t an affiliate code!), if you’re interested in trying.
Supplementation— I use a lot of supplements, honestly, but the few I feel have really helped me are: NAC, magnesium glycinate (esp for the cramping), and turmeric (for overall inflammation management). NAC is a recent one that has been linked to supporting Endo pain, and I feel like it’s helped shorten the duration of my overall pain during my cycles.
Pelvic floor therapy is also super helpful for many people with Endo pain, as it often creates pelvic floor dysfunction and patterns of pain.
Understanding my cycle, and cycle-syncing my foods whenever possible! This post explains it more!
Advil. Sometimes there’s only so much you can do, and bless western medicine for making things more tolerable when it’s just too much.
Excision Surgery (NOT Ablation)
Why is it important to have excision and not ablation?
Excision is cutting out the disease, whereas ablation is topically burning it. Think about an iceberg: there is far more below the surface of the water than above it, and excision is like cutting it out as far as it penetrates the tissues, and ablation is more like just burning off the surface. Aside from not getting all the diseased tissue, cauterization/burning often creates more inflammation in the tissues— and seeing as how Endometriosis is a disease that THRIVES off inflammation, you don’t exactly want to add more inflammation on in your body if you can help it.
Is Endo excision a permanent treatment?
No — simply put, there is no definitive “cure” for Endometriosis (and please run away from any doctor that says a hysterectomy or pregnancies are a cure for Endo!!). Similar to cancer, a treatment like excision surgery can potentially remove all of the existing Endometriosis found in your body, however, there is no way to guarantee or know if it will recur and spread again. This is why you want a surgeon that will thoroughly excise everything they can find, to give you the best outcome that currently exists.
Was this your first surgery?
This was my first surgery and I very much hope my last. This is why I was extremely set on finding an experienced Endo specialist who performs excision surgery— to give myself the best chance at having a surgery done by a thorough surgeon who would do their best to find and excise all the Endo from all of my organs. It makes me sad to know that so many women have had to have multiple surgeries simply from from being led astray by doctors less experienced with Endo, undergoing ablation procedures or incomplete surgical experiences because their surgeons weren’t equipped to excise Endo from trickier areas like the bowels, bladder, and ureters.
Insurance
Did insurance cover your surgery?
Yes, but this was not my first attempt at it. I feel SO fortunate to have been able to access surgery with an experienced excision surgeon and have it be covered by insurance— however, there’s more to this story:
I first attempted to have this surgery in 2021 back in NYC. The only qualified excision surgeon I could find and trusted at the time was out-of-network with insurance (as the vast majority unfortunately are). This is a common problem, so I was advised to seek an “out of network exception” with my insurance. After going through an arduous application appeals process, insurance denied my surgery, saying it was “medically unnecessary, due to lack of proof of diagnosis.” The irony is, is that you have to have the surgery first, in order to get a biopsy of suspected tissue in order to have a confirmed diagnosis. They then directed me to a list of in-network doctors (all of whom only performed ablation and advised BCP as a way to treat Endo…), and said they'd consider an appeal on their decision if treatment with one of those doctors didn’t work.
I knew that I was hoping to have excision surgery this year, so we intentionally chose an insurance plan with better coverage this year (and I ensured that the surgeon I had my eye on was in-network with this plan), and I aggressively pursued reaching my deductible (through lots of acupuncture!), in order to pay less out of pocket when the time came.
On average, excision surgery with an expert MIGS (minimally invasive gynecologic surgeon) can cost $15,000-$25,000.
ACOG, the American Congress of Obstetricians and Gynecologists, also has woefully outdated guidelines for the treatment of Endometriosis, which adversely affects people’s access to treatment because of insurance companies leaning on those outdated guidelines to deny effective treatment like excision treatment.
Recovery (+ recommendations!)
What to expect with surgery recovery?
I REALLY wish I had a better answer for you than this (because I know I was dying for one, and it gets fatiguing telling everyone in your support system that asks that you have zero idea what to expect)— but every person’s recovery is different. I’ve read wildly different accounts of recovery, so I prepared for the worst, and hoped for the best. I would say that I’ve had a fairly optimal recovery thus far, minus a few bumps in the road, but I’m also only 3 weeks out, and I haven’t had a period yet since. Some people experience improved symptoms (especially energy) right away, and some others say they didn’t feel normal for 6 months. I think it also depends on how long this disease has caused you pain, how deep and infiltrating it is on your organs, and your pain tolerances too. Here are some things I can definitively offer though:
The first few days, the GAS pain is often the most uncomfortable. During laparoscopic surgery, they inflate your abdomen with gas, so that they can maneuver around your organs to search for Endo. This gas takes a few days to leave your body, and many people actually feel a lot of shoulder pain from this, because the gas presses up on a nerve in your torso that refers to your shoulders. You want to try to walk around the house a little bit to help move the gas out of your body, so don’t be on full bedrest!
Don’t be a hero, take your pain meds and your stool softeners.
Rest and not pushing yourself is key to a better recovery.
Your first 1-3 period cycles may actually be worse— this varies for people, but once again, I’m prepared for the worst, but hoping for the best.
You might have weird nerve pains… everywhere, and I mean everywhere. Talk to your doc about how to best manage this.
What to bring to the hospital: pillow for the car ride home (to put under your seatbelt to cushion your abdomen), a bucket or plastic bag in case you get nauseous in the car ride home from the anesthesia, a snack for post-op if you have the appetite, change of underwear, socks, phone charger. Leave all your jewelry and valuables at home!
Your recommendations for things to have around the house, post-op?
Peppermint tea— this helps with your gas pains and digestion. Drink it religiously.
Heating pads— this one for your neck and shoulder helped me immensely with soreness from the gas pains, and then I’d also use it flat on my stomach.
Have lots of pillows on hand to prop up under your knees and incline your back for sleep, as it will be nearly impossible to get comfortable otherwise— especially the first week. Some people like a wedge pillow, but I was fine with just stacking pillows.
Optional: a picker-upper and/or a cane. Some people recommended this — bending over to pick things up is indeed horrible for the first week, so if you don’t have a caretake you can ask to do these things, I’d imagine the picker-upper is very helpful. The cane, I didn’t find I needed, but it would be helpful for support overall and maneuvering around!
What is your plan to manage your Endo moving forward, post-op?
Pretty much continuing a lot of the management habits I’ve integrated into my life! Eating well and avoiding the foods I know my body experiences inflammation with (gluten, dairy, excess sugar), good sleep, hoping for more exercise now that I can hopefully engage my core pain-free soon, staying on top of my hormonal health with things like my TCM herbs, and acupuncture when accessible. I’m also beginning pelvic floor therapy soon, as chronic pain can really do a number on your body’s functions, even after disease is gone— because your body is so used to patterns of pain. There’s no guarantee my Endo won’t come back, but I will be doing my best to continue best practices AND hopefully live my life a little more than I was able to before!
Additional Resources on Endo:
WEBSITES
Endo Found— This is the foundation that was founded by the Endo specialist I first saw in NY. Their website has a lot of information and resources on the disease, finding a specialist, education, research, and a lot more.
Nancy’s Nook — Please take this resource with several grains of salt: I personally ignore the most of the posts and personal anecdotes themselves, because you can go down a serious rabbit hole that is more anxiety-inducing than helpful, and Nancy + the moderators can often be snide and insensitive. I only recommend utilizing the group for their resources they share, such as their “Nook-approved excision surgeons,” as a good jumping-off point for your research if you are seeking surgeons.
BOOKS
The Doctor Will See You Now by Tamer Seckin — this book by the NY doctor I initially saw made me feel very understood and helped me learn more about the disease through a doctor’s eyes.
Know Your Endo by Jessica Murnane — a really empowering book for those struggling to mentally come to terms with this disease and managing it.
Vagina Problems by Lara Parker— finally read this book this year, and it’s a great personal read full of humor, honesty, and reality of living with Endo and associated pelvic pain issues. It will make you feel seen.